Why the Best Place to Check Blood Pressure May Be at Home
The numbers taken at a doctor's office can be unreliable. Find the most accurate home monitors here, and learn how to get your pressure under control.

You probably know that high blood pressure (aka hypertension) is a top risk factor for some of the most common and deadliest medical emergencies, including heart attacks and strokes. Consistently high pressure can damage the tissue inside your arteries, leading to plaque buildup and reducing blood flow to your heart and brain.
But measuring your blood pressure accurately can be tricky. In fact, when you get it taken in a doctor’s office, there’s a good chance those numbers won’t reflect your real blood pressure on an ordinary day. Raj Padwal, MD, a professor of medicine at the University of Alberta who runs a specialty hypertension clinic, says that he generally doesn’t ask for in-clinic blood pressure readings for his patients "because 50 percent of the time they’re inaccurate."
There are a few reasons that readings taken in a doctor’s office can be misleading. But the good news is that there’s an easy and relatively inexpensive way to get an accurate picture of your blood pressure from the comfort of your own home.
The Problem With Doctor's Office Blood Pressure Checks
Blood pressure is exquisitely sensitive, changing from moment to moment. It’s "affected by emotional status, mental health, physical activity, ambient temperature, medications, whether you ate, whether you slept well, and on and on," Padwal says.
This vital sign is measured with two numbers: systolic pressure, the top number, which represents the pressure on your arteries as your heart contracts; and diastolic pressure, the bottom number, representing the pressure on your arteries when your heart is at rest.
Best Blood Pressure Monitors
See CR’s reviews of blood pressure monitors at any price and those for $50 or less.
Why Home Blood Pressure Monitoring Works So Well
When you measure at home, you can buy a high-quality monitor with a cuff that fits your arm. You can also be sure to prepare properly and use the correct procedure. And you can take multiple measurements on different days—and provide that data to your doctor.
Monitoring blood pressure at home is especially valuable for anyone whose in-office readings indicate high blood pressure and for those at an elevated risk for heart disease because of preexisting health conditions like diabetes, Padwal says. It can also be useful for tracking the effect of a new medication or an adjusted dosage, or for people who are pregnant or postpartum and should be on the lookout for a severe form of high blood pressure called preeclampsia.
And not only can home monitoring be more accurate than in-office checks, but some studies have found that it can actually help you control your blood pressure, particularly in the first few months of using a monitor.
Choosing a Blood Pressure Monitor
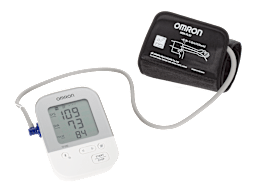
Buying an accurate home blood pressure monitor is key. While most manufacturers haven’t published the results from any accuracy testing, some medical groups have compiled lists of devices that have been validated by independent experts. All of the experts we talked with recommended the American Medical Association’s US Blood Pressure Validated Device Listing as a good starting point when shopping for a home monitor.
CR also rates BP monitors. Our accuracy tests, which we pattern after industry standards, involve comparing each monitor’s readings with the results from the gold standard, a device called a mercury sphygmomanometer. We also evaluate each monitor’s ease of use and comfort. CR members can access our ratings here.
Home blood pressure monitors come in two main varieties: those that are placed on your upper arm and those that go on your wrist. In general, experts (and CR) recommend arm monitors, which tend to be more accurate because there’s less room for error in how they’re positioned.
But using the correct arm cuff size is crucial in getting accurate readings, and some people with larger arm circumferences may not be able to find an arm monitor with an appropriate cuff size. In those cases, wrist monitors can be a good alternative. You’ll just need to take extra care to position them correctly. None of the wrist monitors in CR’s tests scored high enough to earn our recommendation, but several still earned very good accuracy scores.
You may wonder if an alternative to buying your own blood pressure monitor is to use a blood pressure kiosk in your pharmacy. But Padwal says very few public blood pressure kiosks have been validated by independent experts. Plus, it might be challenging to follow guidelines for taking blood pressure correctly when you’re in the middle of a busy pharmacy.
Got High Blood Pressure? Read This.
High blood pressure usually has no symptoms, so people taking medications for it may not see immediate benefits. That makes it hard for many to stick with their meds, Krumholz notes.
But the treatments for hypertension, including both medications and lifestyle changes, can successfully lower your blood pressure. Work with your doctor to find the strategy that works best for you. Here’s what to consider:
Try the DASH diet. The Dietary Approaches to Stop Hypertension, or DASH, is an eating plan that can help lower your blood pressure (and your LDL cholesterol, another risk factor for cardiovascular disease). Rigorous studies have shown that people who followed the DASH plan had lower blood pressure levels at the end of several weeks than people who followed more typical American diets. The DASH diet offers a lot of flexibility and is based on a few simple principles:
• Eating lots of fruits, vegetables, whole grains, fish, poultry, beans, nuts, seeds, vegetable oils, and low-fat dairy.
• Limiting sources of saturated fats like fatty meats and full-fat dairy, as well as sweets and sugary beverages.
• Reducing salt in the diet is also key. When you take in more salt, your body retains more water, which can raise your blood pressure.
Keep in mind that most of our dietary sodium comes not from homemade food but from processed foods and restaurant meals. So focus on reducing those rather than forcing yourself to underseason the food you cook.
Aim for 30 minutes of exercise five days a week. Regular physical activity helps control blood pressure and reduces your risk of other problems, including heart attacks and strokes, diabetes, and even some cancers. An analysis published in 2023 in the British Journal of Sports Medicine evaluated 270 randomized controlled trials to find out if certain types of exercise were better for controlling blood pressure. Many different types were helpful, the study showed, so pick whichever form you enjoy. But it found the most benefit from isometric wall squats, sometime called wall sits, so consider adding those to your routine.
Consider other lifestyle changes. Smoking doesn’t just increase the risk of lung cancer, it also temporarily raises blood pressure and contributes to the long-term buildup of plaque in arteries. Drinking alcohol is also linked to a greater risk of hypertension. Experts recommend limiting your intake to one drink per day for women and two for men. And public health experts also recommend maintaining a healthy weight, or losing weight if you need to, as another strategy for managing or preventing high blood pressure.
Talk to your doctor about meds. A variety of medications are available for controlling blood pressure, including diuretics, ACE inhibitors, calcium channel blockers, and angiotensin receptor blockers. You may need to try a few different drugs, or a combination of them, to find what’s effective for you, Krumholz says. When to start on meds depends on several factors, but doctors generally begin considering them if your blood pressure reaches 130/80 mmHg, and they’re quicker to recommend them the higher it gets from there.
Editor’s Note: This article also appeared in the January 2024 issue of Consumer Reports magazine.